Tendinopathies are a group of conditions that affect tendons, causing pain and dysfunction due to overuse or abnormal loading patterns. They can develop slowly over time, and their management requires a multifaceted approach, blending load management, exercise progression, and patient education. This article is structured around the key points shared in Physio Edge Podcast 138 by @PhysioDMSilvan, delving into how tendons respond to load, how to manage the condition, and offering a step-by-step guide for healthcare professionals to optimize tendinopathy treatment.
1. Understanding Tendinopathy History: Exploring Load and Injury Progression
The Evolution of Tendinopathy
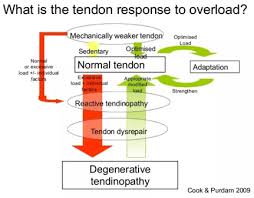
Tendinopathies rarely occur overnight. They are more likely to develop progressively, as the result of cumulative changes in the load a tendon experiences. These changes can be due to:
- Sudden increases in activity levels, such as taking on a new sport or significantly increasing the intensity or frequency of workouts.
- Extended periods of inactivity followed by a rapid return to physical activity (e.g., returning to sports after a break).
- Competitive periods that impose excessive strain without adequate recovery.
Key Clinical Question: When assessing a patient with suspected tendinopathy, it is essential to explore their injury history. Ask about:
- Recent changes in training or activity levels.
- Variations in training surfaces or environments.
- Equipment use (e.g., different shoes or sports gear).
Patients often provide insights into the nature of their injury by recounting the frequency and intensity of their physical activity. This can help the clinician understand the relationship between the load placed on the tendon and the resulting symptoms.
Identifying Fluctuations in Load
The critical element of injury history is understanding load fluctuations over time. Load refers to the physical stress placed on the tendon, which can be influenced by factors such as training volume, intensity, and technique. These load fluctuations can result in microtrauma to the tendon, which, if not managed properly, can progress to tendinopathy.
Example: A runner may increase their weekly mileage by 50%, switch to a new running surface, or change shoes, all of which can impact the load their tendons experience.
Patient Engagement in Load Management
To manage tendinopathy effectively, the patient must participate in understanding their load history. Encouraging patients to recall the types and amounts of activities they’ve engaged in will provide valuable insights and assist in tailoring their rehabilitation program.
2. Contributing Factors to Tendinopathy
Internal and External Contributors
Effective tendinopathy management requires identifying both internal and external factors that contribute to the condition. This enables the healthcare provider to target the right variables during treatment.
Internal Factors
These are generally unmodifiable and include:
- Age: Tendons become less flexible and more prone to injury as people age.
- Gender: Some evidence suggests that hormonal differences, particularly estrogen, may impact tendon structure and healing.
- Metabolic diseases: Conditions like diabetes can impair tendon function.
- Genetic predisposition: Family history can play a role in tendon health.
- Medication use: Fluoroquinolone antibiotics, for example, are known to increase the risk of tendinopathies.
External Factors
These are often modifiable and include:
- Training load: Abrupt increases in volume or intensity can lead to overloading of the tendon.
- Technique: Poor biomechanics or faulty movement patterns may stress certain tendons more than others.
- Training environment: Hard or uneven surfaces can affect the load distribution.
- Equipment: Poorly fitting shoes or equipment (e.g., improper bike setup) can contribute to tendon overload.
Addressing Modifiable Factors
While internal factors may be outside the patient’s control, external factors are typically changeable and should be prioritized in treatment plans. For example, adjusting a patient’s training load, improving biomechanics, or modifying their environment and equipment can significantly reduce stress on the tendon.

3. The Importance of Patient Education
Educating Patients About Tendinopathy
A crucial part of tendinopathy management is educating the patient about their condition. Patients often focus solely on reducing pain, but a successful treatment approach must shift focus towards improving tendon function.
Tendons love load, but how, what, and when to load them becomes key. Patients should understand:
- Delayed symptoms: Tendon pain can manifest hours or even days after activity, making it important to monitor not just immediate symptoms but also delayed reactions.
- Monitoring patterns: Keeping a record of symptoms and activity levels can help identify trends and triggers.
- Pain vs. dysfunction: Pain relief is not synonymous with tendon recovery. The aim is to restore normal tendon function and resilience to prevent recurrence.
Load Management for Self-Monitoring
Patients should learn how to manage and monitor their own symptoms, focusing on:
- The gradual introduction of load to the tendon.
- Exercises that promote healing without exacerbating symptoms.
- Methods to track how activities impact pain and function.
4. Collaborative Approach in Tendinopathy Treatment
Integrating Patient Feedback
Patient engagement in the treatment process is critical for success. Their unique insights into how their bodies respond to exercises and load can shape the treatment plan.
- Local Discomfort: Patients should learn to recognize when and where they should feel local stress or tension during exercises. For example, a patient with patellar tendinopathy should experience discomfort over the patella tendon, which is a normal and expected part of rehabilitation.
- Flexible Options: Providing patients with flexible exercise options that fit their schedule and preferences increases adherence. A personalized approach encourages them to take ownership of their rehabilitation.
- Symptom Diaries: Using a symptom diary to track pain, stiffness, or other issues can help reinforce the connection between exercise and improvements in symptoms.
The best exercises are the ones patients actually do. Adherence is often more critical than selecting the “perfect” exercise.
5. Functional Screening for Tendinopathy
Low-Tech Functional Screening
A simple, low-tech functional screening can help identify problem areas before progressing into more complex sport-specific testing. For example:
- Seated knee extension: Tests knee strength in a controlled, seated position.
- Single leg (SL) decline squat: Focuses on eccentric control and highlights potential weaknesses in the patellar tendon.
- Single leg hop for height or distance: This plyometric test can assess Achilles or hamstring tendons.
By observing symptom reproduction or loss of quality during these tests, clinicians can hypothesize the dominant contributing factors (e.g., strength, endurance, or energy absorption) that need to be addressed.

Monitoring Symptoms in Provocative Tests
Symptom monitoring is essential, especially when dealing with tendinopathy in different regions of the body. For example:
- Achilles tendinopathy: Patients might report morning stiffness or pain that improves with movement.
- Patellar tendinopathy: Decline squats or single leg hops can provoke pain.
- Hamstring tendinopathy: Single leg bridges may reproduce symptoms.
6. Three Key Exercise Parameters for Tendinopathy
1. Maximal Load
The type of exercise (isometric, eccentric, or concentric) is less important than the overall load applied. Tendons thrive on load, and maximal load needs to be a cornerstone of treatment.
2. Isolate the Tendon
Maximal loading should be isolated to the affected tendon. This means exercises must be performed in such a way that compensation through other muscles or joints is minimized.
3. Lengthening the Tendon
Exercises that place the tendon in a lengthened position help improve strength and endurance. Examples include eccentric calf raises for Achilles tendinopathy and Nordic hamstring curls for hamstring tendinopathy.
Exercise Tips:
- Focus on quality over quantity.
- Keep exercises simple but progressive.
- Apply a load at 80-90% of the patient’s capacity to avoid underloading.
7. Keeping It Simple and Achievable
The key to long-term success in tendinopathy management is simplicity and adherence:
- Simple exercises: Exercises like the Spanish squat for patellar tendinopathy are effective and easy to perform.
- Adaptability: Exercises should be progressive but not so complex that they overwhelm the patient. Simple exercises that fit into a patient’s routine are more likely to be performed consistently.
- Gradual progression: Exercises should progress in load, repetitions, or speed without drastic changes to the program.
In conclusion, managing tendinopathies requires a comprehensive and patient-centered approach. By addressing both internal and external contributing factors, educating patients about load management, and employing simple but effective exercises, healthcare providers can guide patients toward recovery and prevention of future issues. Tendons may love load, but it is the how, what, and when that makes all the difference in their rehabilitation.
Thanks for reading
@physiorun